Measurement-Based Care for Improving Mental Health
Mental illness affects millions of people every day. Fortunately, the right tools are available to make evidence-based and more effective mental health treatment possible. Using measurement-based care, providers gain access to the actionable intelligence they can use to more effectively collaborate with patients on care and treatment to achieve the best possible outcomes.
Read on as we take an in-depth look at mental health, explore the need for and value of measurement-based care (MBC), discuss essential tools of MBC, and explain how to put this highly beneficial technique into practice.
Table of Contents
- Part 1: Need for Measurement-Based Care
-
Chapter 1: What is Mental Health? Definition and Key Concepts
-
Chapter 2: Understanding the Role of Measurement-Based Care (MBC) in Behavioral Health
-
Chapter 3: What is the Collaborative Care Model? Application for Mental Health
- Part 2: Tools of Measurement-Based Care
-
Chapter 4: Why Do Medical Providers Use Rating Scales?
-
Chapter 5: Scales for Measuring Mental Health: How They Work
-
Chapter 6: Choosing the Right Measures
- Part 3: Putting Measurement-Based Care into Practice
-
Chapter 7: Measurement-Based Care in the VA: How it Works
-
Chapter 8: Tips for Adopting Measurement-Based Care Within Your Own Practice
-
Chapter 9: What to Consider When Implementing Outcome Measurement Tools
Part 1: Need for Measurement- Based Care
Mental health is a sensitive topic, shrouded in stigma and misinformation. This makes measurement problematic. As such, many patients with mental disorders fail to receive appropriate, timely treatment. By understanding the role measurement-based care and the collaborative care model play in behavioral health, healthcare providers can better identify and care for the mental health needs of their patients.

Chapter 1:
What is Mental Health? Definition and Key Concepts
Mental health is a state of individual wellbeing involving physical, emotional and social actualization, affecting how an individual acts, thinks and feels while also helping them cope with everyday life stresses. Mental health is essential for all life stages, with a primary goal of achieving an absence of mental illness or effectively treating such an illness. According to the Centers for Disease Control and Prevention (CDC), mental health can be negative or positive, while mental illness is a disease. However, among the general public, the two terms often are used interchangeably.
It’s important to note that many mental health issues affect young people, with about 50% of lifetime mental illnesses taking root by the age of 14, and about 75% by the age of 24, according to the National Council of Mental Wellbeing.
Approximately 14% of adolescents in the United States have bipolar or mood disorders, increasing the likelihood of experiencing educational difficulties, engaging in riskier behaviors and even embracing social exclusion. Left untreated, mental illnesses may cause long-term consequences, including psychological impairment and a higher number of school dropouts. Roughly 70% of the youth who are in the juvenile justice system have at least one mental health illness. While the causes of mental illnesses are unknown, psychological and environmental factors significantly contribute to these conditions. Biological factors include nerve cell pathways connecting specific brain regions, defects or injuries in particular brain areas, genetics and infections. Environmental factors might include loss of loved ones, neglect, social or cultural expectations, dysfunctional families and inability to relate to peers.
The most common mental disorders include depression, anxiety, bipolar disorder, schizophrenia and other psychoses, as well as obsessive-compulsive disorder (OCD).
Back to Top ↑
Chapter 2:
Understanding the Role of Measurement-Based Care (MBC) in Behavioral Health
Now let’s discuss measurement-based care further. What is it? MBC measures an outcome secondary to an intervention in a prescribed medication, physical realm or surgical procedure. It could also be any number of interventions, such as transcranial magnetic stimulation (TMS) in behavioral health.
In behavioral health, to achieve an expected outcome, MBC follows a process of care that includes:
- Behavioral health screening
- Diagnostic interviewing
- Diagnostic decision-making
- Treatment decision-making
- A series of monitoring events to ensure outcomes
MBC tracks and measures a patient’s improvement over time. Accuracy is vital when dealing with patients, especially when measuring behavioral change. As such, it is important for patients not to miss appointments or fail to follow their doctor’s prescriptions.
For instance, when a patient regularly reports feeling much better after a therapy under MBC, the clinic might repeat the process for several more weeks to achieve a clear outcome. When a patient doesn’t improve, the doctor might use the data collected to make evidence-based changes to prescribed medications and/or therapies. Again, patient participation and engagement is key. When a patient feels unwell but fails to show up to follow-up appointments, there is no way to measure an outcome and make necessary adjustments.
There are several challenges when using MBC, but the major one remains that most health providers do not apply the approach consistently, especially to behavioral health. Uniformly using the method isn’t just a matter of frequency but also sequencing.
That said, when done properly, MBC benefits both the provider and the patient. Measurement-based practices contribute to clear and concise quantification of beginning point, progress and outcome, making it easier to communicate status among multiple care providers and across settings of care, as is desired with a collaborative care model.
Back to Top ↑

Chapter 3:
What is the Collaborative Care Model? Application for Mental Health
The collaborative care model is a treatment method for mental illnesses that integrates psychological and physical healthcare in a familiar setting. This care model helps address the wide gap in mental health treatment attributed to financial constraints, therapy-seeking stigma and a shortage of behavioral health professionals. The treatment environment includes school-based facilities and primary care clinics, effectively taking mental health therapy where needed.
Collaborative care entails interprofessional cooperation — healthcare and medical experts working together to treat patients. Benefits of such collaboration include:
- Enhanced teamwork with psychiatrists, nurses, radiologists, social workers and other experts authorized to recommend patient care
- Increased payment incentive from the Centers for Medicare & Medicaid Services (CMS)
- More comprehensive care stemming from diverse medical and healthcare professionals working together
- Enhanced patient-care quality from the team effort made by expert professionals, hence offering ongoing care
- Improved communication
Collaborative healthcare in mental health improves efforts to correlate and simultaneously treat mental disorders, lung problems, cardiovascular disease, immunological function and physical pain. Below are examples of collaborative care in mental health:
- Accountable care
- Personalized team care
- Evidence-based care
- Population-based care
There are many promising approaches to measuring health, and clinicians who pursue a collaborative care model benefit from incorporating questionnaires and rating scales into care plans to help with screening, assessing and monitoring mental health. These instruments offer objective, comparable data across care settings and patient populations over time.
Primary healthcare professionals, psychiatrists, managers and therapists collaborate to provide treatment and assess patients’ progress over time. This concept effectively reduces treatment costs of various mental health illnesses across multiple locations, utilizing different payment structures.
Back to Top ↑
Part 2: Tools Used in Measurement-Based Care
Many providers in the behavioral health setting rely heavily on unstructured interviews to guide treatment. Yet seeking information this way can be time-consuming, make it difficult to compare outcomes over time or across settings and can yield unreliable information and data. Rating scales that support measurement-based care can help overcome these and many other behavioral health challenges.

Chapter 4:
Why Do Providers Use Rating Scales?
Several rating scales are helpful in measurement-based care, but some of the most common in behavioral health include the following:
(MINI) Mini-International Neuropsychiatric Interview
The MINI has several versions available and assesses 17 of the most common adult mental health disorders and 24 most common pediatric conditions. The standard and individual versions of the MINI drill down into each disease more specifically. Physicians use a flow chart to help determine which version of the scale would be most appropriate for specific patients. The clinician asks the patient a series of branching no/ yes questions to establish the presence and frequency of symptoms. The standard MINI interview takes approximately 35 minutes to complete.
(SDS) Sheehan Disability Scale
The SDS measures functional impairment across three domains: social, work/school and family life. It’s based on self-report using a 10-point scale from 0 to 10. Patients rate to what extent the symptoms they experience have disrupted their lives in five domains: not at all (0), mildly (1-3), moderately (4-6), markedly (7-9) and severely (10).
(S-STS) Sheehan-Suicidality Tracking Scale
The S-STS survey collects patients’ responses to 14 questions on a rating scale from 0 (not at all) to 4 (extreme). The scale assesses the seriousness of suicidal thoughts, intent, plans, hallucinations, impulses, preparatory behaviors and suicide attempts. The scale can be used as a clinician-administered rating scale or patient self-report to record ideation and behaviors.
Rating scales have several benefits. Most notably, they:
- Provide quantitative measurement to a patient’s experience;
- Offer consistent and comparable means to monitor individual progress during treatment over time;
- Allow clinicians to identify when care interventions are making progress and hence recognize earlier when change may be needed;
- Give enough information for research to derive valuable insights as researchers work to identify best practices;
- Facilitate use of consistent and abundant data to compare patient data at a population level;
- Organize population health data to inform payers about value of care delivered at the system level; and
- Help providers use a measurement-based care process to formulate a more precise care plan.
Read more about the benefits and applications of measurement-based care at “A Tipping Point for Measurement-Based Care,” which provides a detailed literature review.
Back to Top ↑

Chapter 5:
Scales for Measuring Mental Health: How They Work
To effectively illustrate the power of using questionnaires and scales, consider several applications related to body dysmorphic disorder (BDD). According to Cleveland Clinic, BDD is a disorder where preoccupation with an imagined or very slight defect with one’s body can affect an individual’s ability to attend school, work or function in social or home settings. Clinicians use a mix of questionnaires and scales to screen, assess and monitor the progress of BDD patients.
Screening
The Body Dysmorphic Disorder Questionnaire (BDDQ) is available for researchers, clinicians and those patients who wonder if they have BDD. The questionnaire takes up to 5 minutes to administer and assists in identifying patients that require further diagnosis using the BDD Diagnostic Module. BDDQ versions cater to teens and adults. The questionnaires’ responses have no comparative element as opposed to rating scales since they are either yes or no.
Assessment
The assessment provides patients and providers with an indication of the severity or frequency of symptoms. The Body Dysmorphic Disorder Diagnostic Module, also known as BDDD, is based on the DSM-5 diagnostic criteria for BDD. It evaluates appearance preoccupations and repetitive behaviors of clinical significance, uses specifiers to identify patients with either insight specifiers or muscle dysmorphia, and aids differentiation from an eating disorder.
Monitoring
To identify changes in patient health with treatment, a clinician uses another type of scale, such as the Yale-Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder (BDD-YBOCS). BDD-YBOCS is an example of a scale used commonly to measure the progress of patients diagnosed with BDD. The scale features a series of 12 semi-structured items to assess the severity of BDD during the previous week and asks patients to respond to and rate items. They rate these items like “I check my appearance (e.g., in mirrors, by taking photos of myself or by touching with my fingers)” or “I avoid situations because of my appearance.”
The clinician can identify whether the patient’s health worsens or improves when comparing patient data from week to week over time. Tracking health this way over a period — especially when viewed across patient populations — aids clinicians and researchers in identifying which interventions support best outcomes and developing effective evidence-based practices.
Back to Top ↑
Chapter 6:
Choosing the Right Measures
Devising the right system for measurement in mental healthcare is challenging but vital for health screening, assessment of treatment progress and monitoring whether maintenance of patient progress is evident. The proper measures aid researchers in identifying whether an intervention is of value to particular populations. Data also helps decrease unwarranted variation in care treatment and diagnosis, which, according to Wolters Kluwer, accounts for at least 25%, and possibly up to 65%, of the unnecessary costs in care delivery.
The Importance of Outcome Measures in Mental Healthcare: Key Things to Know
Importantly, focusing on outcome versus process measures can provide valuable insights for improving mental health. Process measures focus on an action that a patient or physician performs at a given point in time. For instance, a patient process-measure could be taking medication while a physician process-measure could be recording temperature or administering a blood test. Process measures tell only a part of the story, focusing on what was performed and not the outcome. Outcome measures differ from process measures in that they explain the results of steps taken. Using behavioral health outcome measures, a physician can determine the deterioration or improvement of patient conditions when changes occur and better ensure treatment has its intended effect. Data from outcome measures also helps with quality monitoring and tracking progress at the aggregate level.
How are Mental Health Outcomes Measured?
In behavioral health, outcome measures are necessary because they indicate whether patients are improving due to the treatment, and both patients and providers can track and report outcome measures. Patient outcome measures are collected through patient-self reporting that typically involves completing forms, with results called “patient-reported outcomes measures (PROMs)” or “patient-reported symptom rating.” According to the National Institutes of Health (NIH), mental health outcome measures must be reliable and valid, sensitive to change, comparable across relevant client service types and groups, and meaningful to clinicians and their clients.
A wide range of mental health outcome measures helps gauge the patients’ mental wellness. Some standard outcome measures in behavioral health include cognitive performance, physical and social activity, and behavioral experiences.
An outcome-based approach to mental health is beneficial to providers, patients, healthcare systems and society in the following ways:
- Enables providers to track and monitor patient potential backsliding and improvements
- Offers meaningful insights into the patient’s state of mind
- Assesses clinical effectiveness of the healthcare system and providers
- Demonstrates desired changes occurring from a patient’s perspective
- Helps procure funding and support payment
Back to Top ↑
Part 3: Putting Measurement-Based Care Into Practice
Healthcare providers routinely use measurement to determine physical health. However, according to Psychiatric Online, only 18% of psychiatrists and 11% of psychologists apply a rating system during their routine mental healthcare practices.
Yet despite infrequent use in behavioral health, measurement-based care is a proven, powerful tool to improve treatment outcomes. It is no wonder that it's beginning to draw greater attention as of late. One of the most notable projects is use within the nation’s most extensive integrated healthcare system: the Veterans Health Administration, a U.S. Department of Veterans Affairs (VA) component.

Chapter 7:
Measurement-Based Care in the VA: How it Works
Measurement-based care is impacting mental health outcomes within the VA. The VA has been rolling out MBC principles to establish a behavioral health standard in treatment planning and setting recovery goals.
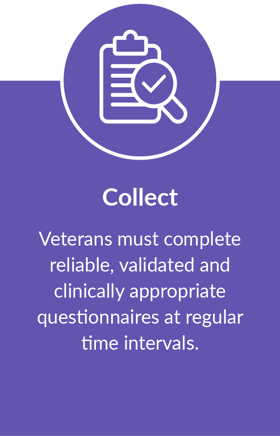
Measurement-based care for behavioral health at the VA uses a “collect, use and share” foundation that works as described below:
When the VA initiated its MBC in mental health initiative, an interagency task force on veterans and military agreed to an initial pilot of four measures for the measurement-based care program. The four measures are:
- (PCL-5) PTSD Symptom Checklist for PTSD assessment
- (BAM-R) Brief Addiction Monitor for substance use and risk together with recovery factors assessment
- (PHQ-9) Patient Health Questionnaire for depression assessment
- (GAD 7) Generalized Anxiety Disorder for anxiety assessment
After the pilot, the VA conducted a survey comprising 230 mental health providers across nearly 50 VA medical centers. The study aimed to assess attitudes and self-reported use of various measurement-based care components. The adoption of the MBC tools at the VA was high: about 58% of the providers recorded collecting at least one measure for at least half of their patients and provided positive feedback on using such utility.
The survey revealed a high acceptance of treatment planning, with 72% indicating that they always explained their results to the patients while 65% used the results as part of shared decision making. However, only 37% indicated using scores when discussing a patient with another healthcare provider.
The authors of the VA pilot program study note measurement-based care using patient-reported data shows improved treatment outcomes for patients with mental illness, from better engagement to faster response to treatment. Yet, despite these benefits of MBC and the availability of validated measures for use specifically by mental health practitioners, the approach is still adopted to a lesser degree than in other clinical areas.
The VA also acknowledges that the adoption of measurement-based care is lower in mental healthcare because it is a “pretty big adjustment” in clinical practice. As a result, the VA is rolling out MBC in phases to study the best ways to put it into practice.
Back to Top ↑

Chapter 8:
Tips for Adopting Measurement-Based Care Within Your Practice
Approaches to transitioning toward measurement-based care vary. Some providers find it useful to think about the data they are using in different categories and then stagger adoption.
As Dr. Jennifer Birdsall, chief clinical officer for CHE Behavioral Health Services, notes in “Understanding Outcome Measurement: Mental Health Experts Share Insight,” sometimes it’s helpful to first think about data as a means to be collaborative with patients about their care, looking for opportunities to discuss particular measures as a signal of whether symptoms are getting worse or improving.
As comfort with this data use grows, then focus can begin to include making use of aggregate data applications. Birdsall notes this trend information can be invaluable: “I can look at it as, ‘We have really good outcomes for depression and anxiety, but for our patients with substance abuse disorders, we don’t. Why is that? Do we need to look at our programming?’ These insights are really impactful to me as a clinical leader.”
Back to Top ↑

Chapter 9:
What to Consider When Implementing Outcome Measurement Tools
Implementing outcome measures alone does not improve patient care. Rather, clinicians must establish systems that guide usage. Here are some tips on how you can better implement measurement-based care within your organization:
- Use digital solutions; for instance, you can screen, assess and track patients more seamlessly using software programs
- Incorporate an outcome-measures approach in communicating progress
- Integrate process improvement consistently to make collaboration on patient health decisions easier
Also, check out Proem, which provides a variety of tools for incorporating measurement-based care into behavioral health practice. Proem’s solutions support data collection to track each patient’s health journey and validate outcomes for providers, payers and researchers.
Back to Top ↑




.png)